THE HEART AND ARRHYTHMIAS
Function, components and functioning of the heart
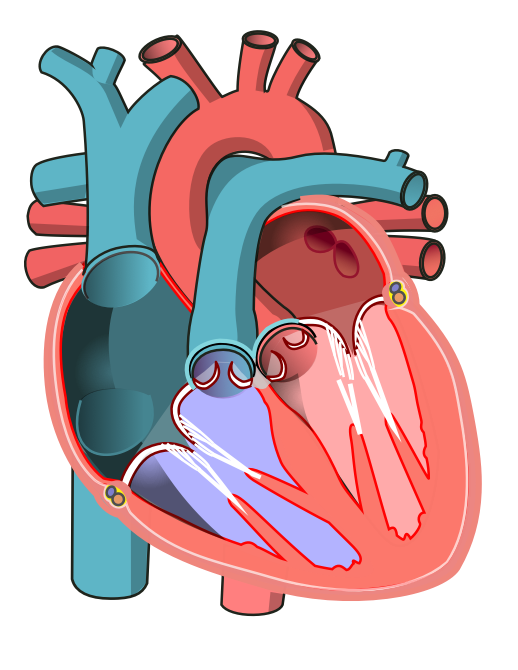
The heart is located in the chest, protected by a framework of cartilage and bones (sternum, ribs and vertebrae) called the ribcage. It is like a hollow muscle about the size of a pepper and divided into four compartments; two upper (atria) and two lower (ventricles).
For blood to circulate in our body, the heart acts as a natural pump. It allows blood to flow, carrying oxygen and other nutrients to our organs and tissues. On the other hand, it collects waste and carbon dioxide from the whole body so that they can be eliminated.
Actually, they are like two bombs, one right and one left. Each of them has an upper part called the atrium, whose function is to store blood and then pass it to the lower part, called the ventricle, which is really the part of the heart that pumps blood. The right part is responsible for collecting the blood already used and with little oxygen to send it to the lung to recharge with oxygen. This oxygenated blood reaches the right side of the heart to be pumped and distributed throughout the body.
Under normal conditions, the rhythm of the heart is set by a small area located in the upper part of the right atrium, called the sinus node and is our natural pacemaker. There, a small electrical impulse is spontaneously generated and distributed throughout the heart, traveling rapidly through specialized high conduction tissues and through the heart’s own muscle cells.
It first spreads through the left and right atria, which contract, ejecting blood from inside them into the ventricles. When the two ventricles have been filled, they contract, expelling a large part of the blood they contain into the right lung and the left towards the rest of the body. At rest the heart usually contracts between 60 and 100 times per minute.
Slow heart rate – Pacemaker therapy
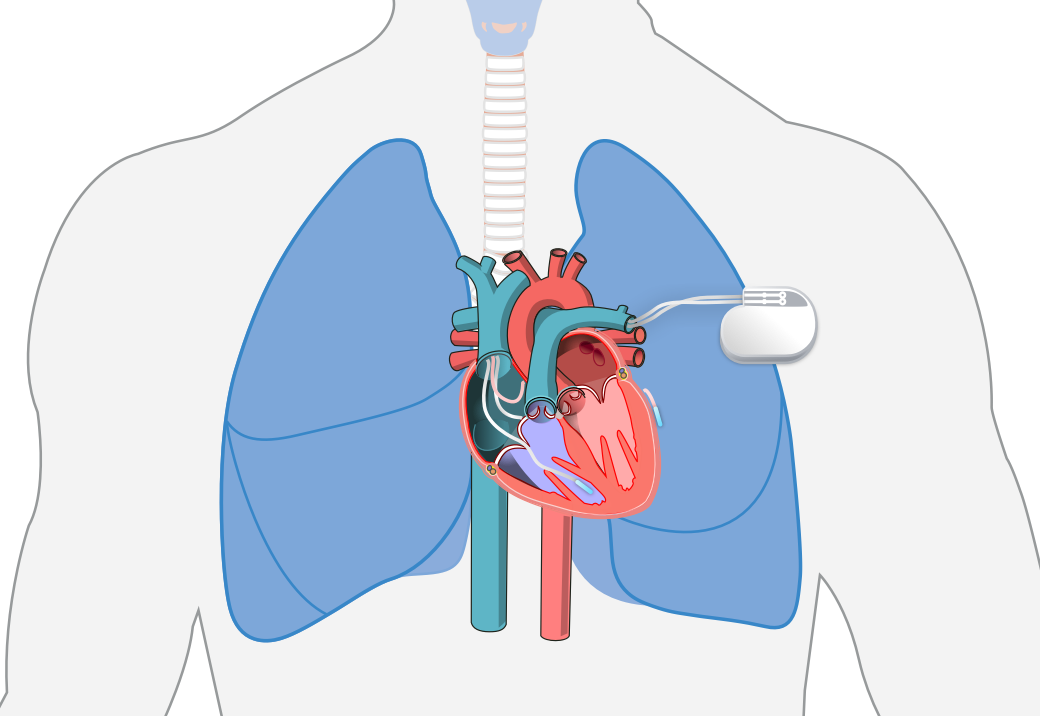
A slow heart rate (bradycardia) is defined as a rate less than 60 beats per minute. If the heart is unable to pump enough blood to the body because it beats too slowly, implantation of a pacemaker may be considered.
Why does bradycardia occur?
There are several reasons that can cause bradycardia, but some of the most frequent are failure of the sinus node (the heart’s natural pacemaker), or failures at the level of conduction of the electrical impulse between the atria and ventricles. These conditions produce pauses in the heart rhythm that sometimes generate symptoms such as syncope, dizziness or heart failure.
What is the pacemaker for?
Electrical impulses are sent by the pacemaker device to tell your heart to contract and produce a heartbeat. Most pacemakers work just when they’re needed – on demand. It helps the heart pump blood at a proper rate by sending electrical signals when necessary. In this way, an adequate supply of blood to the rest of the body is maintained.
Fast Heart Rate – ICD Therapy
Sometimes the heart can speed up to very high rates. This is called tachycardia, and depending on the origin of this rapid rhythm, the consequences can be fatal. To avoid this, the implantation of an ICD (Implantable Cardioverter Defibrillator) can be considered.
Why does tachycardia occur?
There are many origins for tachycardia, but not all of them are detrimental to health. Ideally, in situations where your body requires an extra supply of oxygen, the heart speeds up to meet that demand. This happens when you exercise, in stressful situations, or when faced with certain strong emotions, for example. This is called sinus tachycardia, it originates in the atrium and does not pose any health risk.
On the other hand, there are tachycardias whose origin is the ventricle itself. They are called ventricular tachycardias (or tachyarrhythmias) and these can have serious consequences for the patient
What is the ICD used for?
Ventricular tachycardia
It is a fast but regular rhythm, which usually originates from a specific site and which generates symptoms such as a feeling of lack of oxygen, palpitations or dizziness. In these cases, the ICD will send a sequence of electrical impulses at a rate faster than the tachycardia itself. This is done to “win” over your own heart and take control in order to return to a normal rhythm. This type of therapy is called antitachycardia pacing (EAT).
Ventricular fibrillation
It’s a fast and chaotic pace. It originates from several points in the ventricle at the same time, and in these cases the heart can beat so fast that, on a practical level, it would be as if it were stopped, causing loss of consciousness or even cardiac arrest. In these cases, the ICD will deliver a high-energy shock, “resetting” the heart cells to try to regain a normal rhythm.
Heart Failure – Resynchronisation therapy
Heart failure is a disease with very diverse origins, which generates a lot of discomfort in the patient who suffers from it. HF is characterized by a loss in muscle strength, which makes the heart unable to pump enough blood to the body. This decrease in blood flow increases the blood pressure in the heart and causes symptoms such as tiredness, fatigue and fluid accumulation in the lungs and extremities, among others. In addition, these patients usually present an alteration in the conduction system, which causes a loss of synchrony between the right and left ventricle, reducing the efficiency with which the heart is capable of pumping blood. One option to treat this disease is the implantation of a pacemaker or resynchronizing ICD (CRT-P or CRT-D). These devices are the same as those mentioned above, but a lead is added to the left ventricle. In this way, it is possible to recover the synchrony between both ventricles and therefore increase the capacity of the heart to pump blood effectively.
Heart with arrhythmias curable with ablation therapy
Some arrhythmias have their origin in certain cells of the heart that behave differently than expected. The most common cases are:
-
- Cells that should not conduct electrical impulses (they work as an insulator), in some people present conduction, and the impulse can propagate in unwanted ways.
- Areas that present an exacerbated electrical activity and can come to dominate the natural rhythm coming from the sinus node (natural pacemaker).
- Regions of the heart affected by different pathologies that produce new stimulation cycles (reentry circuits).
In these cases, the arrhythmia can be cured by destroying the cells that exhibit inappropriate behavior or by creating a lesion that cuts off the circular conductions to prevent their perpetuation. The process of destroying heart cells is called cardiac ablation, and different energy sources can be used to achieve this goal. Some of them are the use of radiofrequency (heat) or nitrous oxide for cryoablation (cold). Another recently incorporated technique is electroporation, in which high-energy electrical pulses are sent to the affected area with an ablation catheter. This catheter is inserted into a vein/artery in the leg (femoral) and is followed to the heart. The amount of energy and the type of catheter used will depend on the patient’s anatomy, the affected area and the objective of the ablation. This method has a very high success rate, completely curing the arrhythmia in some cases.
Living with an ICD
Currently, the technology of these devices means that there are very few limitations for the patient who wears the ICD.
-
Appliances
Household appliances do not pose a risk to the ICD carrier. Any appliance such as hair dryers, dishwashers, TV, razor, computer, drills can be used normally. The exception to this are induction cookers, which can interfere with the ICD, so it is recommended to keep a distance of 60 cm from them.
- Mobile
Mobile phones do not pose a risk to the patient at a distance of 15 cm from the device. To maintain safety, it is enough to talk on the phone on the opposite side of the ICD and not keep it in the jacket pockets near the chest.
- Sport
The ICD does not pose a risk to the practice of any sport at an electrical level. However, certain precautions must be taken when playing contact sports such as rugby, basketball or soccer. The practice of sports alone (swimming, sailing, running…) is not recommended due to possible dizziness or fainting.
- Travel
Certain precautions must be taken during security checks at airports. ICD patients must always carry the card that identifies them as ICD carriers. With this identifier, you will avoid going through the metal detector, which affects the operation of the device.
- Hospitals
You should always notify healthcare personnel that you are an ICD carrier. They will know how to proceed in case you need to do any procedure that may affect the operation of the device.
- Driving
The regulations on driving vehicles for patients with ICDs can be found in Spanish legislation. The most important thing you should know is that you cannot drive any vehicle until 3 months after implantation if you are a secondary prevention patient and 1 month if you are a primary prevention patient. If you have received a shock for the device, you will also have to wait 3 months until you can drive. On the other hand, there are limitations for patients with heart disease. It is recommended to consult with your cardiologist for more detailed information.